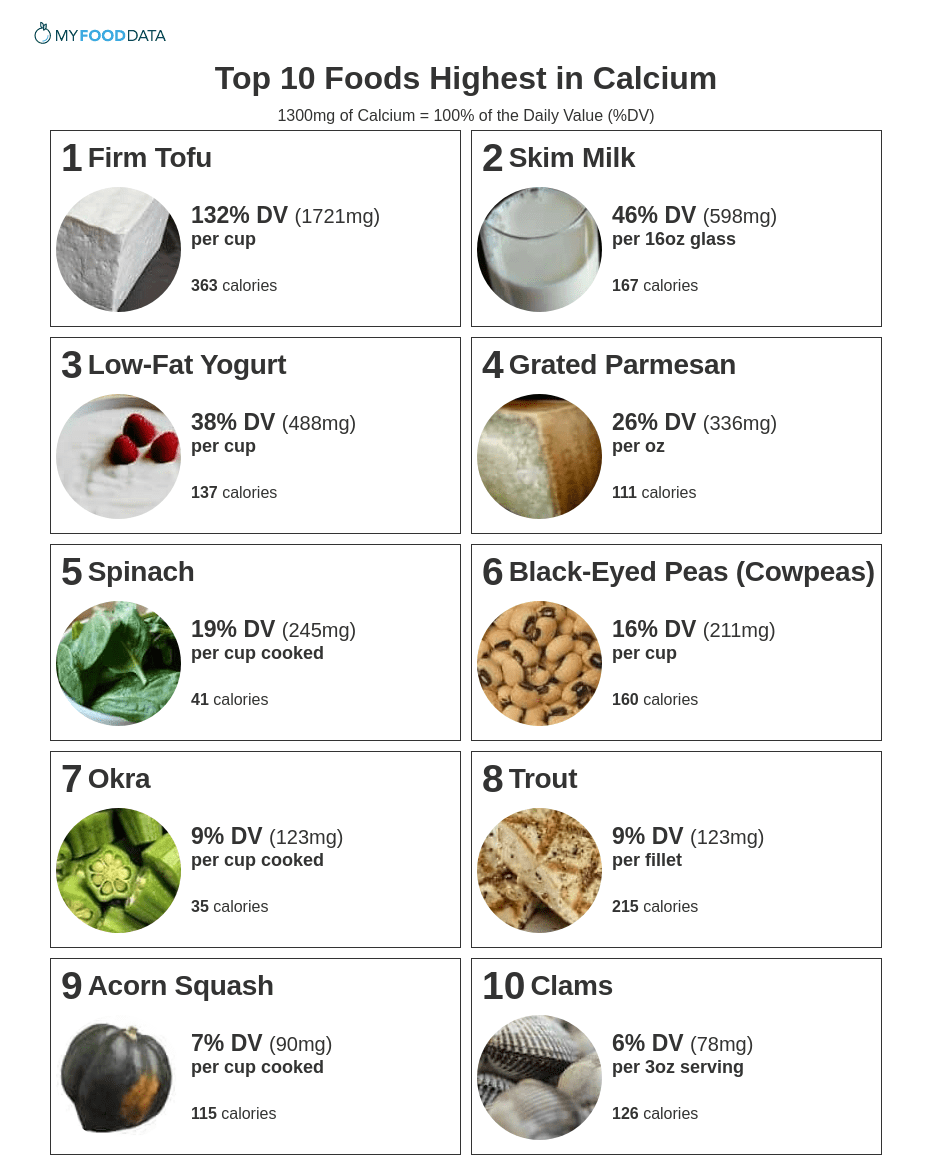
Top 10 Foods Highest in Calcium

Calcium is a mineral necessary for the growth and maintenance of strong bones, strong teeth, nerve signaling, muscle contraction, and secretion of certain hormones and enzymes. (1,2,3,4)
Calcium is an electrolyte, and a deficiency in calcium can lead to numbness in the fingers and toes, muscle cramps, convulsions, lethargy, loss of appetite, and abnormal heart rhythms. (5,6) A long-term calcium deficiency can lead to bone loss (osteopenia) and fragile bones (osteoporosis). (7) Vitamin D and Vitamin K are also important nutrients for preventing osteoporosis. (7)
Excess calcium (particularly from supplements) can lead to constipation and kidney stones. (8) In certain populations, calcium supplementation has been shown to increase the risk of vascular diseases like stroke and heart attack. (9,10)
High-calcium foods include tofu, milk, yogurt, cheese, leafy greens, beans, clams, okra, trout, and acorn squash. The daily value (DV) for calcium is 1300mg. (11,12)
Evidence suggests that phytic acid and oxalic acid in beans and greens can hinder calcium absorption. However, some green vegetables and beans are still good sources of calcium. (13,14) Further the calculated daily value (DV) already takes into account absorption and bio-availability. (12) For more info, see the section on calcium absorption.
Below is a list of high calcium foods ranked by common serving size, for more see the nutrient ranking of over 200 foods high in calcium. Also see the lists of high calcium vegetables, and high calcium fruits.
Foods High in Calcium
-
 1. Firm Tofu + Add
1. Firm Tofu + Add
Calcium
per CupCalcium
per 100gCalcium
per 200 Calories1721mg
(132% DV)683mg
(53% DV)949mg
(73% DV)Only tofu prepared with calcium sulfate is high in calcium. Most tofu will provide between 10% - 40% DV calcium per cup. Check ingredient labels.
-
 2. Skim Milk + Add
2. Skim Milk + Add
Calcium
per 16oz GlassCalcium
per 100gCalcium
per 200 Calories598mg
(46% DV)122mg
(9% DV)718mg
(55% DV)Whole Milk and Low Fat 2% Milk provide 42-45% DV per 16oz glass. Fortified Soymilk also provides up to 46% DV per 16oz glass.
See all dairy foods high in calcium.
-
 3. Low-Fat Yogurt + Add
3. Low-Fat Yogurt + Add
Calcium
per CupCalcium
per 100gCalcium
per 200 Calories488mg
(38% DV)199mg
(15% DV)711mg
(55% DV) -
 4. Grated Parmesan + Add
4. Grated Parmesan + Add
Calcium
per OzCalcium
per 100gCalcium
per 200 Calories336mg
(26% DV)1184mg
(91% DV)604mg
(46% DV)Other Cheeses High in Calcium
- 26% in 1/2 cup of low-fat ricotta
- 26% DV in 1oz of parmesan
- 22% DV in 1oz of gruyere
- 19% DV in 1oz of Swiss cheese
- 10% DV in 4oz of cottage cheese
See all dairy foods high in calcium.
-
 5. Spinach + Add
5. Spinach + Add
Calcium
per Cup CookedCalcium
per 100gCalcium
per 200 Calories245mg
(19% DV)136mg
(10% DV)1183mg
(91% DV)Other Leafy Greens High in Calcium
- 21% DV in 1 cup of cooked collards
- 15% DV in 1 cup of turnip greens
- 13% DV in 1 cup of Scotch (curly) kale
- 5% DV in 1 cup of cooked broccoli
Note: Oxalates in leafy green vegetables impair calcium absorption. Studies on the effect of oxalates are mixed. (13,14) In general, leafy greens as part of a balanced diet are a good source of calcium.
See the list of high calcium vegetables.
-
 6. Black-Eyed Peas (Cowpeas) (Boiled and Drained) + Add
6. Black-Eyed Peas (Cowpeas) (Boiled and Drained) + Add
Calcium
per CupCalcium
per 100gCalcium
per 200 Calories211mg
(16% DV)128mg
(10% DV)264mg
(20% DV)Other Beans High in Calcium
- 20% DV in 1 cup of cooked green soybeans
- 12% DV in 1 cup of white beans
- 10% DV in 1 cup of navy beans
Note: The black-eyed peas listed above show a high calcium number since they were measured after being boiled and drained. Draining yields more beans per cup and a higher calcium number. See this comparison of 6 different brands of black-eyed peas vs the USDA official number. Most commercial brands of black-eyed peas provide 80-120mg of calcium, or 6-9% DV, per cup (not drained).
See all beans high in calcium.
-
 7. Okra + Add
7. Okra + Add
Calcium
per Cup CookedCalcium
per 100gCalcium
per 200 Calories123mg
(9% DV)77mg
(6% DV)700mg
(54% DV)See the list of vegetables high in calcium.
-
 8. Trout + Add
8. Trout + Add
Calcium
per FilletCalcium
per 100gCalcium
per 200 Calories123mg
(9% DV)86mg
(7% DV)115mg
(9% DV)More Fish High in Calcium
- 15% DV in a 3oz can of salmon
- 10% DV in a 6oz pike fillet
- 9% DV in a 5oz trout fillet
See all fish high in calcium.
-
 9. Acorn Squash + Add
9. Acorn Squash + Add
Calcium
per Cup CookedCalcium
per 100gCalcium
per 200 Calories90mg
(7% DV)44mg
(3% DV)157mg
(12% DV)See the list of vegetables high in calcium.
-
 10. Clams + Add
10. Clams + Add
Calcium
per 3oz ServingCalcium
per 100gCalcium
per 200 Calories78mg
(6% DV)92mg
(7% DV)124mg
(10% DV)Other Seafood High in Calcium
- 12% DV in 3oz of cuttlefish
- 9% DV in 1 cup of blue crab
- 7% DV in 3oz of octopus
- 6% DV in 3oz of lobster
- 6% DV in 3oz of shrimp
See all fish high in calcium.
Printable One Page Sheet
How Much Calcium Do You Need Everyday?
The daily value (%DV) for Calcium is 1300mg and is a general target intended for most people. The Recommended Daily Allowance (RDA) shows specific targets by age and gender. The RDA for Calcium is between 800mg - 1300mg for most people.
| Life Stage | RDA |
|---|---|
| Children | |
| 1-3 years old | 700mg |
| 4-8 years old | 1000mg |
| Males | |
| 9-18 years old | 1300mg |
| 19-70 years old | 1000mg |
| 70+ years old | 1200mg |
| Females | |
| 9-18 years old | 1300mg |
| 19-50 years old | 1000mg |
| 50+ years old | 1200mg |
| Pregnancy | |
| 14-18 years old | 1300mg |
| 19-50 years old | 1000mg |
| Lactation | |
| 14-18 years old | 1300mg |
| 19-50 years old | 1000mg |
What Affects Calcium Absorption?
- Amount of Calcium In Your Body - When previous consumption of calcium is low, your body will naturally absorb more calcium to compensate for the difference. (15)
- Vitamin D Intake - Vitamin D is critical for the absorption and regulation of calcium. (16,17) It can be found in foods or created by exposing skin to sunshine.
- Age - Calcium absorption declines with age, particularly for women over 70 and men over 50. (18,19)
- Pregnancy - Pregnant women absorb more calcium. (20)
- Phytic and Oxalic Acid - The absorption of calcium from foods low in oxalates and phytic acid can be 20-40% as is true for milk and kale. (21,14) While oxalic acid and phytic acid does hinder calcium absorption it does not block it altogether. For example, 5% of the calcium in spinach is absorbed (22), while 30% of the calcium in soybeans is absorbed (23). Still avoiding foods high in phytic and oxalic acid will benefit calcium absorption. High amounts of oxalic acid are found in plant foods like spinach, collard greens, sweet potatoes, rhubarb, and beans. Phytic acid is found in whole bread and wheat bran.
Should I Take Calcium Supplements?
Unless prescribed by a doctor or health care provider calcium supplementation may do more harm than good. (24,25)
Major concerns with the over-consumption of calcium include gastrointestinal disease, kidney stones, and even heart disease. (24,25)
Only take calcium supplements if directed by a doctor or health care provider, or if you are sure you are consuming less than the recommended 1000-1200mg per day.
Further, calcium supplements will not be effective without adequate intake of vitamin D. (16,17)
What Other Foods and Nutrients Can Help Make My Bones Stronger?
Several nutrients are necessary for strong bones in addition to calcium. These include vitamin D, vitamin K, magnesium, phosphorus, protein, boron, silicon, and fluoride. (26,27,28)
Further, resistance exercises like weight lifting, and even tennis, can help maintain strong bones and encourage bone development or create "osteogenic effects". (29,30,31)
What fruits and vegetables provide calcium?
Fruits high in calcium include calcium-fortified orange juice, prickly pears, tangerines, oranges, and kiwifruit. They provide between 28mg (2% DV) to 349mg (27% DV) of calcium per serving. See the article for high-calcium fruits.
Vegetables high in calcium include collard greens, spinach, turnip greens, kale, mustard greens, and beet greens. They provide between 55mg (4% DV) - 197mg (21% DV) of calcium per serving. See the article for high-calcium vegetables.
From the Nutrient Ranking Tool
Use the ranking tool links below to select foods and create your own food list to share or print.
- Foods High in Calcium
- Foods Low in Calcium
- Vegetables High in Calcium
- Fruits High in Calcium
- Vegetarian Foods High in Calcium
- Nuts High in Calcium
- Grains High in Calcium
- Beans High in Calcium
- Dairy High in Calcium
- Breakfast Cereals High in Calcium
- Fast Foods High in Calcium
View more nutrients with the nutrient ranking tool, or see ratios with the nutrient ratio tool.
Related
Data Sources and References
- Cashman KD. Calcium nutrition and metabolism Br J Nutr. 2002 May;87 Suppl 2:S169-77. doi: 10.1079/BJNBJN/2002534. 12088515
- Hanioka T, Ojima M, Tanaka K, Aoyama H. Low calcium intake is related to increased risk of tooth loss in men Gerodontology. 2007 Jun;24(2):87-92. doi: 10.1111/j.1741-2358.2007.00166.x. 17518955
- Ren ZL, Zuo PP. Calcium signalling: A common target in neurological disorders and neurogenesis J Pharmacol Sci. 2012;120(3):139-45. doi: 10.1254/jphs.12r06cp. Epub 2012 Oct 26. 23099323
- Steinberg JP, Leitner JW, Draznin B, Sussman KE. Calcium calmodulin and hormone secretion Diabetes. 1984 Apr;33(4):339-45. doi: 10.2337/diab.33.4.339. 6200377
- [No authors listed] Electrolytes Ann Clin Lab Sci. 2022 May;52(3):511-525. 35777803
- Palal B, Sinsakul M, Reutrakul S. Hypocalcemia in Malignancy - Unexpected but Common Case Rep Endocrinol. 2011;2011:370583. doi: 10.1155/2011/370583. Epub 2011 Oct 29. 22937282
- Murray TM. Importance of calcium, vitamin D and vitamin K for osteoporosis prevention and treatment CMAJ. 1996 Oct 1;155(7):935-9. 8837543
- Reid IR, Bolland MJ. Controversies in medicine: the role of calcium and vitamin D supplements in adults Nutrients. 2020 Apr 7;12(4):1011. doi: 10.3390/nu12041011. 32272593
- Muscogiuri G, Barrea L, Altieri B, Di Somma C, Bhattoa HP, Laudisio D, Duval GT, Pugliese G, Annweiler C, Orio F, Fakhouri H, Savastano S, Colao A. Vitamin D and Calcium Supplements: Helpful, Harmful, or Neutral for Cardiovascular Risk? Curr Vasc Pharmacol. 2019;17(6):610-617. doi: 10.2174/1570161117666190408165805. 30963976
- Heravi AS, Michos ED. Calcium and Vitamin D Supplementation. Myths and Realities with Regard to Cardiovascular Risk Methodist Debakey Cardiovasc J. 2019 Jul-Sep;15(3):207-213. doi: 10.14797/mdcj-15-3-207. 31687100
- U.S.FDA - Daily Value on the New Nutrition and Supplement Facts Labels
- Aloia JF. Dietary Reference Intakes for Calcium and Vitamin D J Clin Endocrinol Metab. 2011 Oct;96(10):2987-96. doi: 10.1210/jc.2011-0090. Epub 2011 Jul 27. 21795456
- Heaney RP, Weaver CM. Calcium absorption from kale Am J Clin Nutr. 1989 Oct;50(4):830-2. doi: 10.1093/ajcn/50.4.830. 2801588
- Sotelo A, González-Osnaya L, Sánchez-Chinchillas A, Trejo A. Effects of fiber, phytic acid, and oxalic acid in the diet on mineral bioavailability Int J Food Sci Nutr. 2010 Feb;61(1):29-39. doi: 10.3109/09637480903213649. 20001762
- Bronner F. Nutritional aspects of calcium absorption J Cell Biochem. 2003 Feb 1;88(2):387-93. doi: 10.1002/jcb.10330. 12520541
- Fleet JC, Reyes-Fernandez P. Vitamin D-Mediated Regulation of Intestinal Calcium Absorption J Steroid Biochem Mol Biol. 2020 Jun;200:105670. doi: 10.1016/j.jsbmb.2020.105670. Epub 2020 Apr 10. 32283207
- Lorenzo Sellares V, Torregrosa V. Vitamin D, calcium homeostasis and aging Nefrologia. 2008;28 Suppl 3:67-78. 19018742
- Sørensen OH, Lumholtz B, Lund B, Lund B, Hjelmstrand IL, Mosekilde L, Melsen F, Bishop JE, Norman AW. Impaired vitamin D metabolism with aging in women. Possible role in pathogenesis of senile osteoporosis J Clin Endocrinol Metab. 1982 Jun;54(6):1258-61. doi: 10.1210/jcem-54-6-1258. 6978888
- Lorenzo Sellares V, Torregrosa V. Age-related decline of bone mass and intestinal calcium absorption in normal males Nefrologia. 2008;28 Suppl 3:67-78. 19018742
- Gillies BR, Ryan BA, Tonkin BA, Poulton IJ, Ma Y, Kirby BJ, St-Arnaud R, Sims NA, Kovacs CS. Pregnancy up-regulates intestinal calcium absorption and skeletal mineralization independently of the vitamin D receptor J Bone Miner Res. 2018 Jan;33(1):16-26. doi: 10.1002/jbmr.3217. Epub 2017 Aug 2. 28686309
- Murray TM. Calcium bioavailability and its relation to osteoporosis CMAJ. 1996 Oct 1;155(7):935-9. 8837543
- Weaver CM, Heaney RP. Calcium absorbability from spinach Calcif Tissue Int. 1991 Oct;49(4):244-7. doi: 10.1007/BF02556212. 1760767
- Jariwalla RJ. Soybean phytate content: effect on calcium absorption Am J Clin Nutr. 1992 Sep;56(3):609. doi: 10.1093/ajcn/56.3.609. 1503078
- [No authors listed] Calcium supplements: benefits and risks J Intern Med. 2016 Mar;279(3):311. doi: 10.1111/joim.12474. 26891945
- Daly RM, Ebeling PR. The good, the bad, and the ugly of calcium supplementation: a review of calcium intake on human health Nutrients. 2010 May;2(5):505-22. doi: 10.3390/nu2050505. Epub 2010 May 17. 22254038
- Gennari C. Essential Nutrients for Bone Health and a Review of their Availability in the Average North American Diet Public Health Nutr. 2001 Apr;4(2B):547-59. doi: 10.1079/phn2001140. 11683549
- Francis RM. The role of nutrients in bone health, from A to Z Br J Nutr. 2008 Jan;99(1):155-9. doi: 10.1017/S0007114507791924. Epub 2007 Jul 19. 17640420
- Chachra D, Limeback H, Willett TL, Grynpas MD. The effects of fluoridated water on bone strength J Dent Res. 2010 Nov;89(11):1219-23. doi: 10.1177/0022034510376070. Epub 2010 Sep 21. 20858781
- Fagundes Belchior G, Kirk B, Pereira da Silva EA, Duque G. Effects of Resistance Exercise on Bone Health Eur Geriatr Med. 2020 Oct;11(5):715-724. doi: 10.1007/s41999-020-00355-6. Epub 2020 Jul 16. 32676865
- Calbet JA, Dorado C, DÃaz-Herrera P, RodrÃguez-RodrÃguez LP. Bone mineral content and density in professional tennis players Med Sci Sports Exerc. 2001 Oct;33(10):1682-7. doi: 10.1097/00005768-200110000-00011. 11581552
- Guadalupe-Grau A, Fuentes T, Guerra B, Calbet JA. The effects of progressive resistance training on bone density: a review Sports Med. 2009;39(6):439-68. doi: 10.2165/00007256-200939060-00002. 19453205
Simplify Nutrition Tracking with MyFoodData!
Speedy Tools and Detailed Data FREEEasily analyze your meals to find the best foods for your goals.
✅ Use our recipe nutrition calculator and nutrition comparison tool.
✅ Access expert nutrition data tools and in-depth articles.
✅ Log foods and organize your recipes with a free account.


 Next ➞
Next ➞
